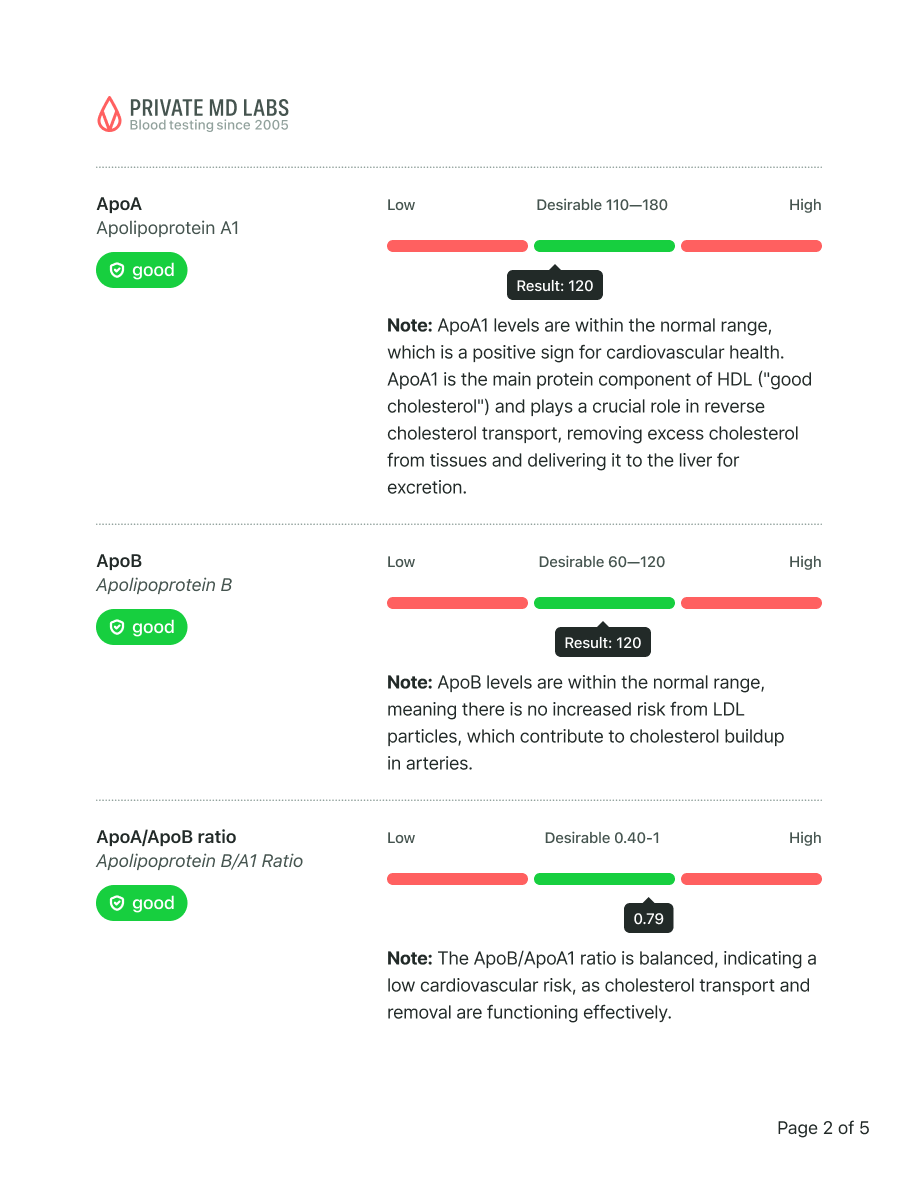
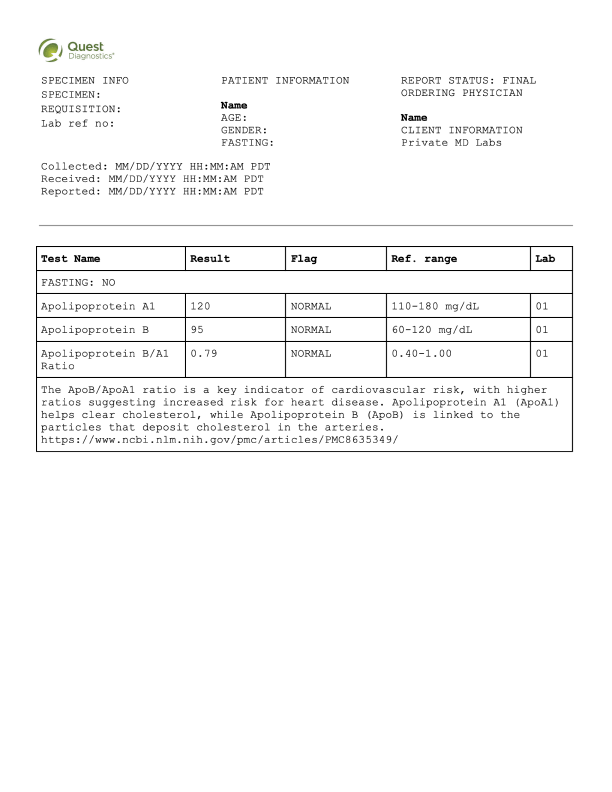
Sample results
Methylmalonic acidemia is a rare genetic metabolic disorder that prevents the body from properly breaking down certain proteins and fats. It is caused by deficiency in the enzyme methylmalonyl-CoA mutase or problems with vitamin B12 metabolism, leading to toxic accumulation of methylmalonic acid in blood and tissues. The Methylmalonic Acid blood test is the most important test for diagnosis, as it directly measures the elevated levels characteristic of this disorder.
 90-day money-back guarantee
90-day money-back guarantee
 Lab order in minutes
Lab order in minutes
 Save a trip to the doctor
Save a trip to the doctor
 Low prices since 2005
Low prices since 2005
 Labs within 2 miles
Labs within 2 miles
Methylmalonic acidemia is caused by genetic mutations that affect the enzyme methylmalonyl-CoA mutase or disrupt vitamin B12 metabolism in the body. These inherited defects prevent the normal breakdown of certain amino acids (isoleucine, valine, methionine, threonine) and odd-chain fatty acids, resulting in dangerous accumulation of methylmalonic acid in the blood and tissues. The condition follows an autosomal recessive inheritance pattern, meaning a child must inherit two defective gene copies (one from each parent) to develop the disorder.
The Methylmalonic Acid blood test is the most important test for methylmalonic acidemia because it directly measures the level of methylmalonic acid that accumulates in the bloodstream due to the metabolic defect. People with this genetic disorder show dramatically elevated methylmalonic acid levels, often 100 to 1000 times higher than normal, making this biomarker the gold standard for confirming diagnosis. This test is typically performed during newborn screening or when symptoms suggest a metabolic disorder, and it helps distinguish methylmalonic acidemia from other similar conditions while also monitoring treatment effectiveness over time.
You should get tested if your newborn shows poor feeding, vomiting, lethargy, or failure to thrive in the first days or weeks of life. Testing is also warranted if a child or adult experiences unexplained developmental delays, recurring episodes of metabolic crisis (vomiting, dehydration, lethargy), or has a family history of methylmalonic acidemia. Early diagnosis through blood testing is critical because prompt treatment with a specialized low-protein diet, vitamin B12 supplementation, and medical management can prevent serious complications like brain damage, kidney failure, and life-threatening metabolic crises.
 Save a trip to the doctor, go directly to the lab
Save a trip to the doctor, go directly to the lab
 Instant orders, results often overnight*
Instant orders, results often overnight*
 Results explained in simple language
Results explained in simple language
 Reviewed by US licensed doctors
Reviewed by US licensed doctors
 Fast & confidential, we never sell or share your data
Fast & confidential, we never sell or share your data
 No insurance needed, transparent pricing
No insurance needed, transparent pricing
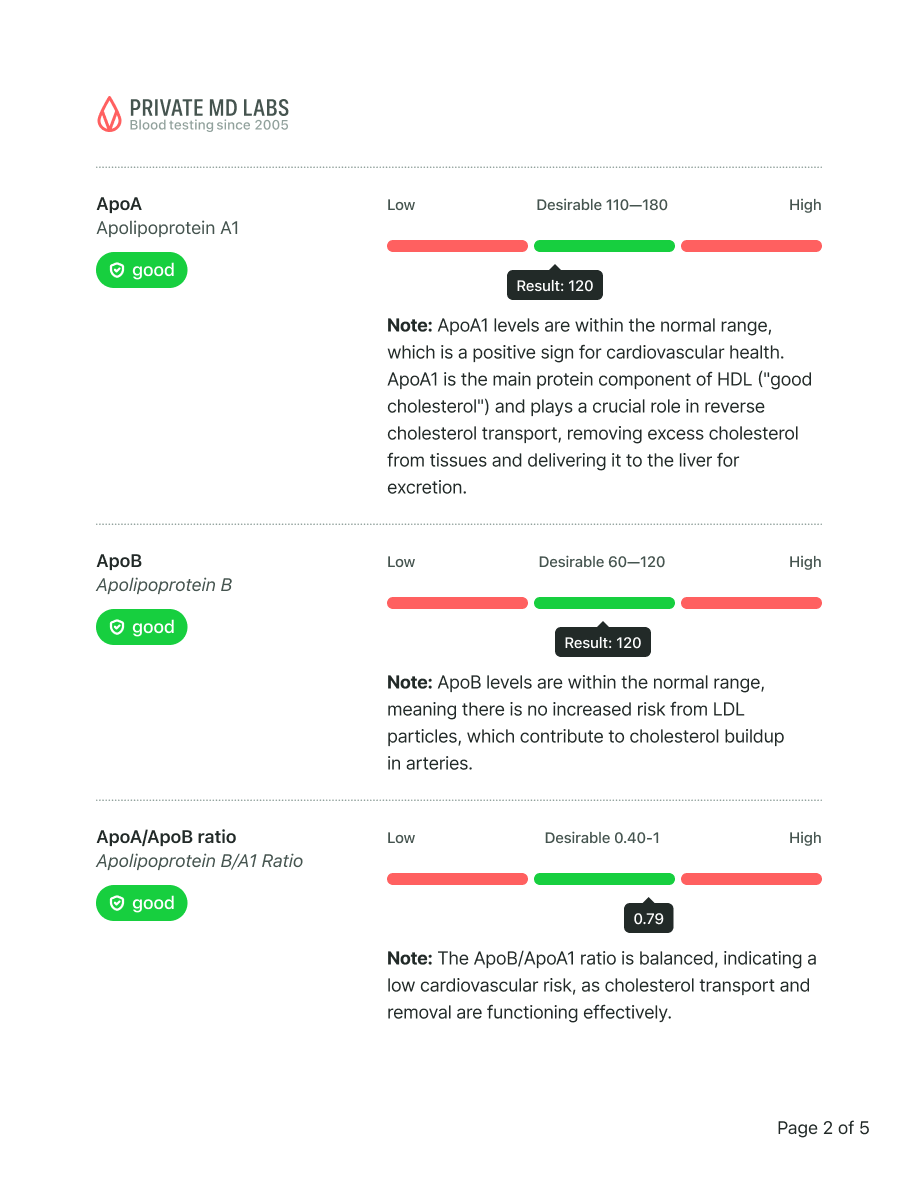
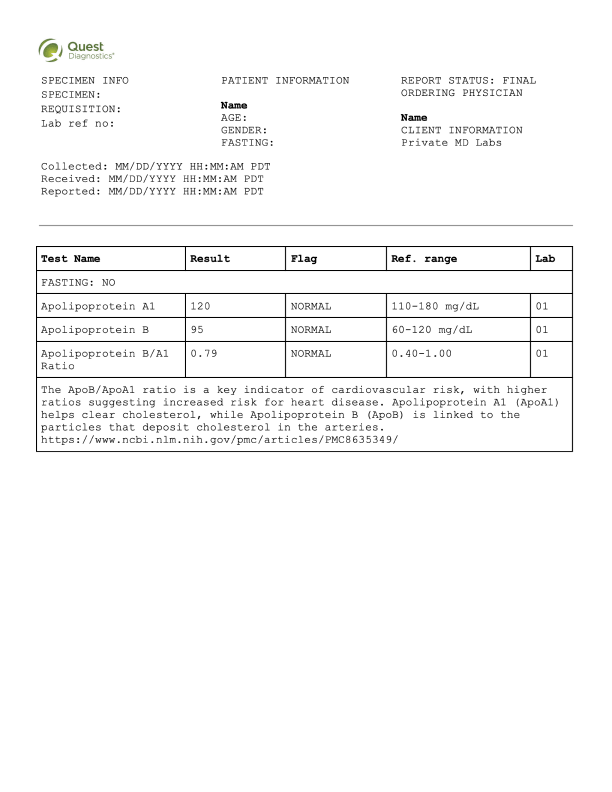
What this means
Your testosterone levels are slightly below the optimal range. While this is not necessarily cause for concern, it may contribute to occasional fatigue, reduced motivation, or lower muscle mass over time.
Recommended actions
Increase resistance or strength training
Prioritize 7–8 hours of quality sleep per night, try to reduce stress
Include more zinc- and magnesium-rich foods (like shellfish, beef, pumpkin seeds, spinach)
Consider retesting in 3–6 months
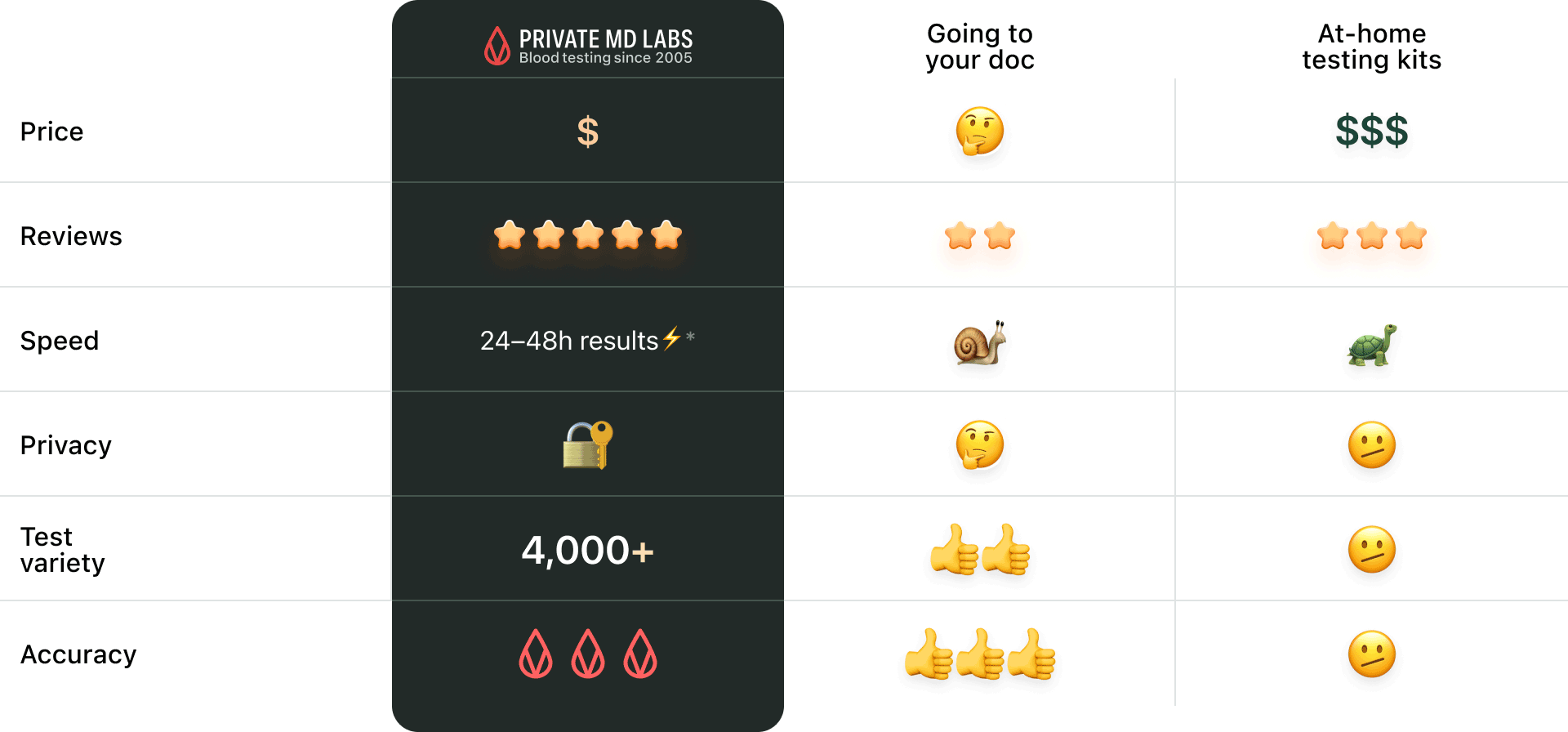
Not overhyped or overpriced. Just comprehensive blood testing made simple and for everyone.






Sample results
Your 24/7 Lab Guide
Quick questions: