Sample results
Disseminated mucormycosis is a rare, life-threatening fungal infection that spreads throughout multiple organ systems in the body. It is caused by fungi in the Mucorales order, particularly species like Mucor racemosus, which invade tissues and blood vessels in immunocompromised individuals. The Mucor racemosus IgG antibody test is the most important test for detecting immune response to this aggressive fungal infection.
 90-day money-back guarantee
90-day money-back guarantee
 Lab order in minutes
Lab order in minutes
 Save a trip to the doctor
Save a trip to the doctor
 Low prices since 2005
Low prices since 2005
 Labs within 2 miles
Labs within 2 miles
Disseminated mucormycosis is caused by fungi in the Mucorales order, most commonly species like Mucor racemosus, Rhizopus, and Rhizomucor. These fungi are found naturally in the environment in soil, decaying organic matter, and compost piles. When inhaled or introduced through broken skin, these organisms invade blood vessels and tissues, spreading rapidly throughout the body in people with weakened immune systems. The infection occurs almost exclusively in immunocompromised individuals whose bodies cannot mount an effective defense against these opportunistic fungi.
The Mucor racemosus IgG antibody test is the most important blood test for disseminated mucormycosis because it detects specific antibodies your immune system produces in response to Mucor racemosus infection. This test measures IgG antibodies in your blood that indicate exposure to or active infection with this dangerous fungal species. While tissue biopsy remains the gold standard for definitive diagnosis, antibody testing provides crucial supporting evidence and can help identify the specific Mucor species involved. Early detection through antibody testing is especially valuable in immunocompromised patients where rapid diagnosis can be life-saving.
You should get tested if you have a weakened immune system and develop sudden fever that does not respond to antibiotics, unexplained facial swelling or sinus pain, persistent headaches with vision changes, cough with bloody sputum, or chest pain with difficulty breathing. Testing is especially urgent if you have diabetes with poor blood sugar control, are undergoing chemotherapy for cancer, have recently received an organ transplant, are taking high-dose steroids, or have experienced severe burns or trauma. Because disseminated mucormycosis progresses extremely rapidly and has a high mortality rate, immediate testing and medical evaluation are critical at the first sign of symptoms in high-risk individuals.
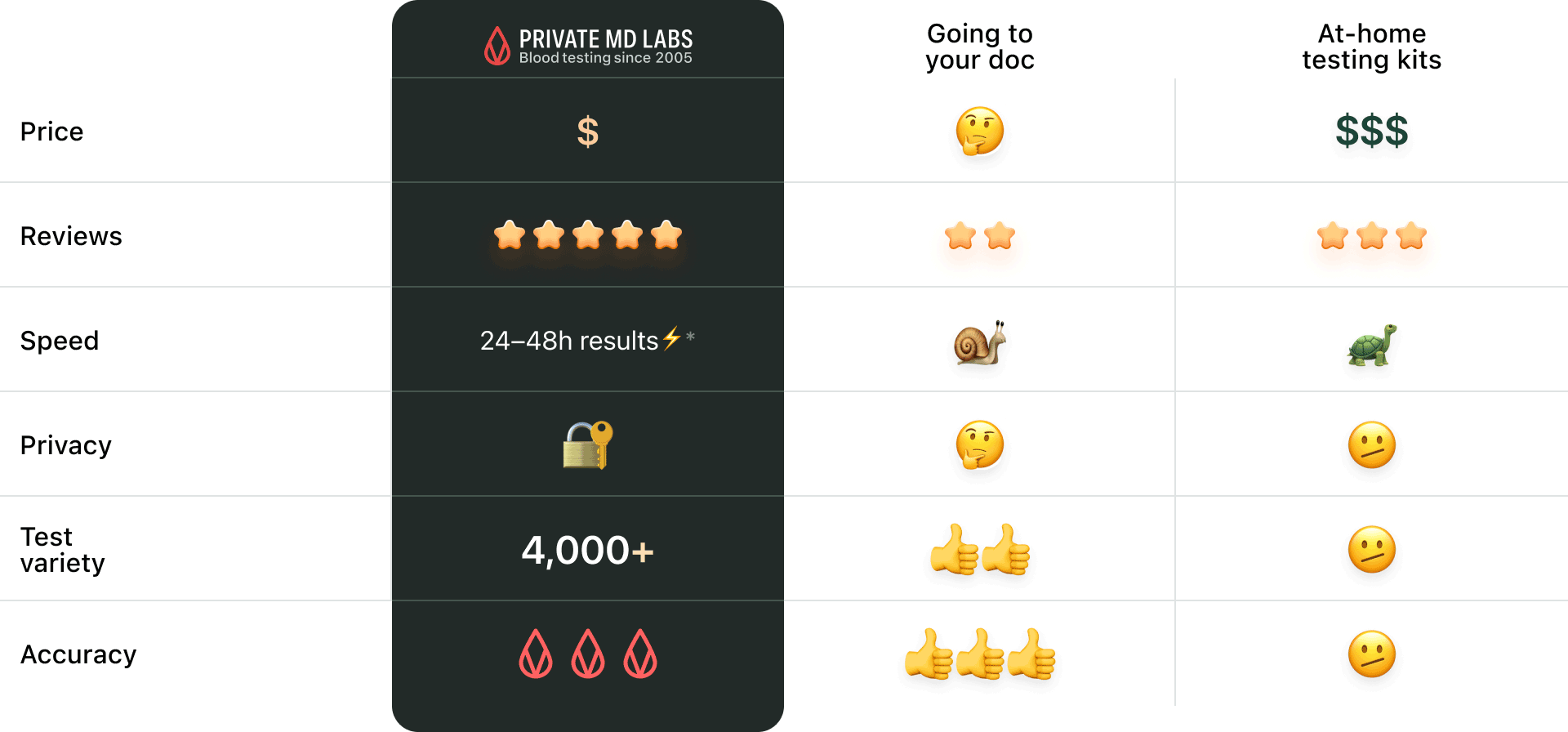
 Save a trip to the doctor, go directly to the lab
Save a trip to the doctor, go directly to the lab
 Instant orders, results often overnight*
Instant orders, results often overnight*
 Results explained in simple language
Results explained in simple language
 Reviewed by US licensed doctors
Reviewed by US licensed doctors
 Fast & confidential, we never sell or share your data
Fast & confidential, we never sell or share your data
 No insurance needed, transparent pricing
No insurance needed, transparent pricing
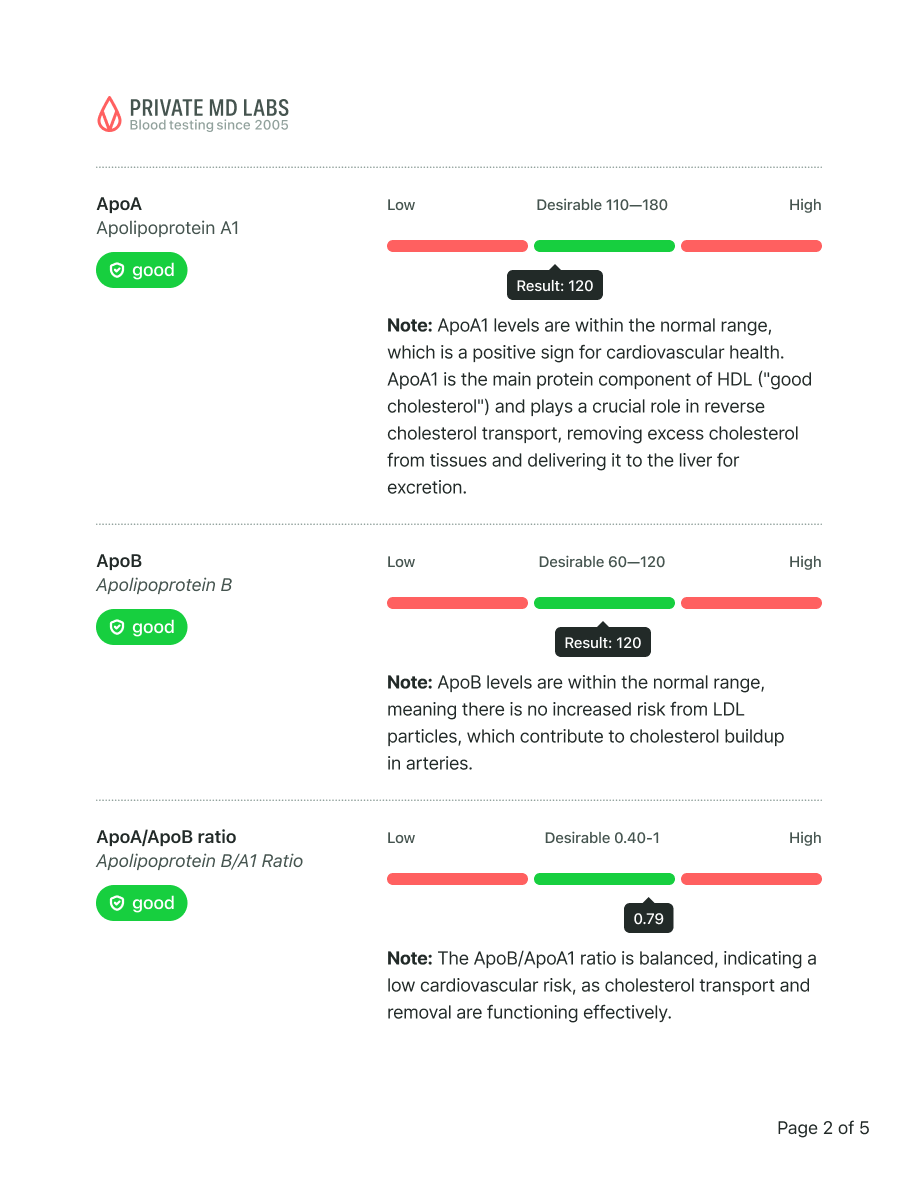
What this means
Your testosterone levels are slightly below the optimal range. While this is not necessarily cause for concern, it may contribute to occasional fatigue, reduced motivation, or lower muscle mass over time.
Recommended actions
Increase resistance or strength training
Prioritize 7–8 hours of quality sleep per night, try to reduce stress
Include more zinc- and magnesium-rich foods (like shellfish, beef, pumpkin seeds, spinach)
Consider retesting in 3–6 months
Not overhyped or overpriced. Just comprehensive blood testing made simple and for everyone.






Sample results
Your 24/7 Lab Guide
Quick questions: